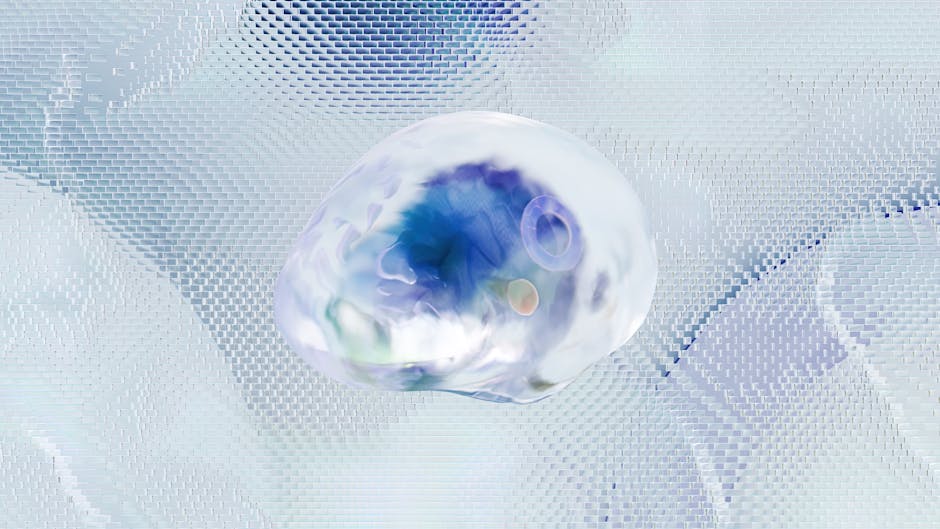
NPH Brain: Understanding Normal Pressure Hydrocephalus and Its Impact on Cognitive Function
Normal pressure hydrocephalus (NPH) is a neurological condition characterized by an accumulation of cerebrospinal fluid (CSF) within the brain’s ventricles. While the pressure of the CSF isn’t necessarily elevated, the excess fluid can lead to a range of debilitating symptoms affecting cognitive function, mobility, and bladder control. Understanding NPH brain changes is crucial for early diagnosis and effective management.
What is Normal Pressure Hydrocephalus (NPH)?
Contrary to its name, NPH isn’t defined by high CSF pressure. Instead, it’s the volume of CSF that’s the primary issue. The ventricles, fluid-filled cavities within the brain, become enlarged, causing pressure on brain tissue. This pressure doesn’t necessarily register as high on a standard spinal tap measurement, hence the ‘normal pressure’ designation. The exact cause of NPH remains largely unknown, though several factors are implicated, including:
- Previous brain injury or surgery: Head trauma, brain bleeds, or prior neurosurgical procedures can disrupt the normal flow of CSF.
- Subarachnoid hemorrhage (SAH): Bleeding into the space surrounding the brain can obstruct CSF pathways.
- Infections: Meningitis or other infections affecting the brain’s membranes can lead to CSF accumulation.
- Genetic predisposition: Although not definitively established, a genetic component is suspected in some cases.
- Idiopathic NPH: In many cases, the underlying cause remains unknown.
Symptoms of NPH: The Triad and Beyond
The classic presentation of NPH involves a triad of symptoms:

- Gait disturbance: This is often the first symptom noticed, characterized by an unsteady, wide-based gait, frequent falls, and a magnetic gait (feet seem stuck to the floor).
- Cognitive impairment: This can range from mild forgetfulness and difficulty concentrating to more severe dementia-like symptoms, including memory loss, disorientation, and executive dysfunction.
- Urinary incontinence: Frequent urination, urgency, and incontinence are common.
However, it’s crucial to understand that not all individuals with NPH will experience all three of these symptoms. Some may primarily exhibit cognitive changes, while others may have predominantly gait problems. The symptoms can also evolve gradually, making diagnosis challenging.

Other symptoms that may be present include:
- Dementia-like symptoms: Including apathy, personality changes, and difficulty with problem-solving.
- Depression: A common co-occurring condition.
- Headaches: Though less common than in other forms of hydrocephalus.
Diagnosing NPH: A Multifaceted Approach
Diagnosing NPH requires a comprehensive evaluation, as the symptoms can mimic other neurological conditions. The diagnostic process typically includes:
- Neurological examination: To assess gait, cognitive function, and other neurological signs.
- Brain imaging (MRI or CT scan): To visualize the ventricles and assess their size. Enlarged ventricles are a key indicator, but not conclusive on their own.
- Lumbar puncture (spinal tap): To measure CSF pressure (though this is often normal in NPH).
- CSF flow studies: More advanced techniques may be used to assess the flow of CSF.
- Neuropsychological testing: To comprehensively evaluate cognitive function.
Treatment Options for NPH
The primary treatment for NPH is often a surgical procedure called a ventricular shunt. This involves placing a small tube (shunt) to drain excess CSF from the ventricles to another part of the body, such as the abdominal cavity. This procedure can significantly alleviate symptoms, particularly gait disturbances and cognitive impairment. However, shunt surgery carries its own risks, and careful consideration is required.
Other treatment options may include:
- Physical therapy: To improve gait and balance.
- Occupational therapy: To adapt daily living activities.
- Speech therapy: To address cognitive and communication challenges.
- Medication: To manage co-occurring conditions like depression or urinary incontinence.
Living with NPH: Coping and Support
A diagnosis of NPH can be life-altering, but with appropriate treatment and support, individuals can maintain a good quality of life. Living with NPH requires a multifaceted approach, including adhering to the prescribed treatment plan, engaging in physical and cognitive therapies, and seeking emotional support. Support groups and counseling can be invaluable for coping with the challenges of the condition.
Conclusion: Early Diagnosis is Key
NPH is a treatable condition, but early diagnosis is crucial for optimal outcomes. If you experience symptoms suggestive of NPH, such as gait changes, cognitive impairment, or urinary incontinence, it’s essential to consult a neurologist. Prompt evaluation and treatment can significantly improve the quality of life for individuals affected by NPH brain changes.

